Personality & Vision Objectives
- It is well established and widely acknowledged that the main criterion for selecting a suitable multifocal patient is his/her willingness to be free from glasses. If your patient does not request independence from glasses and does not mind wearing them, this patient is not suitable for this type of IOL implant. Refractive patients are more likely to notice the photic side effects of multifocal IOLs than regular cataract patients 4,5). Patients that have had previous refractive surgery frequently show additional loss of contrast with a reduction in visual quality 6).
- The person’s dynamics and his/her personality are factors to consider. For instance, a patient who is extremely critical and has very high expectations presents a source of concern. Positive, easy-going patients who understand that a surgical procedure involves risks and are willing to accept compromises on visual acuity in exchange for freedom from glasses, are the ideal candidates.
- Take the patient’s lifestyle into consideration. Are glasses causing inconvenience during activities? For example when swimming, golfing, or switching from reading glasses to no glasses during meetings or presentations. And how important is the visual quality in low light conditions to your patient? There are occupations that make multifocals inadvisable- pilots, drivers, astronomers and anyone whose job requires activity at night or low-light conditions 3).
Next, you can help patients to decide on the best lens model for them, with recommendations based on your pre-op measurements and experience. So, what corneal and eye measurements should be done? Nowadays, there are several different types of equipment that can help achieve accurate pre-operative diagnostics 7).
Pre-op measurements
Which diagnostics should be performed? These days there are several different types of equipment that help us to achieve accurate pre-operative diagnostics 7).
- Dry-eye and meibomian gland dysfunction should be treated pre-operatively.
If present, assess if the dry eye may be impacting the topography. If there is impact, treat the dry eye first and take a new measurement afterwards. If there is no impact on the topography, you can inform the patient of the dry eye and start the treatment.
- Refractive errors after MIOL implantation are a major source of retreatment.
In terms of biometry, optical measurements of axial length are usually accurate and better than ultrasound. Ensure good K reading of the patient’s eye. Consider 4th generation formulas for the calculation of the dioptric power. - Assess the cornea; make sure that the patient does not have a significant corneal cylinder (>1.0 D), depending on the steep axis. The visual acuity at all distances decreases in proportion to the diopters of astigmatism.
- It is important to assess 3rd and 4th order corneal a berrations such as coma as well. Anterior corneal coma values greater than 0.32 μm may result in intolerable dysphotopsia in the presence of a diffractive optics multifocal IOL 17).
- Confirming the normal functionality of the macula and its anatomy is crucial. A test with an optical coherent tomographer (OCT) is advised.
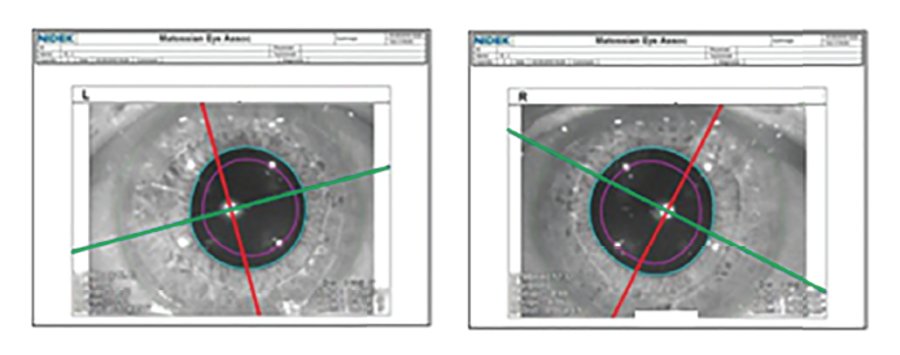
- Other important factors that may influence the final outcome are angle kappa and pupil size 8,9). Centration of the mIOL is critical to achieving maximum optical performance 10). Patients with decentred implants may experience glare, halos and a decline of visual acuity. Angle kappa is the distance between the pupil centre and the visual axis. When the optics of the implant and the optics of the eye align, good outcomes and happy patients are much more likely. A lens can be perfectly centred within the pupil, but the visual axis may not be exactly in the centre of the pupil. The presurgical evaluation of angle kappa helps to identify patients who may not be ideal candidates for a mIOL.
- With the enlarged central zone that can go up to 2.6 mm for far vision, the Precizon Presbyopic NVA model is the best option for a large angle of kappa, compared to other presbyopic IOLS with smaller central zones. Patients with large pupils will be more likely to suffer from glare. The pupil size should not exceed the IOL body diameter of 6.0mm. Patients with small pupils (hence 2.2mm) will benefit less from the segments in the Precizon Presbyopic IOL for far and near, as their vision will be limited to the central area of the IOL.
- Finally, rule out ocular diseases that may predispose future complications (e.g. anterior segment pathology, glaucoma, corneal dystrophy, ocular inflammation, pseudoexfoliation syndrome, retinal disorders).
Counseling patients
There is no best way to counsel patients. Cultural and organizational differences have a large impact on choosing the best approach. We interviewed several specialists from different countries, resulting in a summary of nine steps that may help during the conversations with your presbyopic patients.

Check out the complete Special on Patient Selection & Counseling in PDF »




